, Urinary Urgency and Frequency and Feels Like a Rubber Band Around My Low Back and Groin Area ?
In the spring of 1996, André James* was under a great deal of stress. Married, with a young family to support, he was finishing his medical training at a big-city hospital and anxiously searching for a job. One day, he suddenly experienced severe testicular pain. It was as if someone grabbed both testicles and kept tightening his grip.
*Editor's note: To protect his privacy, the patient's name and some biographical details have been changed. All medical details are as reported. A patient's physicians are usually not named, per editorial policy, but James requested that some be included in this article, and the physicians agreed.
Frightened, James immediately saw a urologist, who examined him, ran several tests, and declared that he could find nothing wrong. But he noted that he often saw police officers, who were under tremendous stress, with the same symptoms. Stress, the physician said, might have triggered James' symptoms, but he prescribed an antibiotic just in case one of the tests had failed to detect a bacterial infection. It took two rounds of antibiotics and several weeks' time, but the pain finally went away. And when James found a job at another hospital, the stress went away, too.
James forgot all about the problem until 2004, when he developed testicular pain again. This time, however, the pain was somewhat different. It moved from one testicle to the other and then migrated above his pubic bone. He urinated frequently, and when he did, he felt as if he were urinating boiling water. His penis hurt, and the pain grew more intense after he had sex. He saw another urologist, who did a complete workup. Once again, the doctor couldn't find any obvious problems, and the laboratory tests all came back negative. The doctor concluded that James had chronic pelvic pain syndrome (CPPS), a type of prostatitis. One possible cause: excessive tightness in the muscles of the pelvic floor (see Figure 1).
Figure 1: Pelvic floor muscles
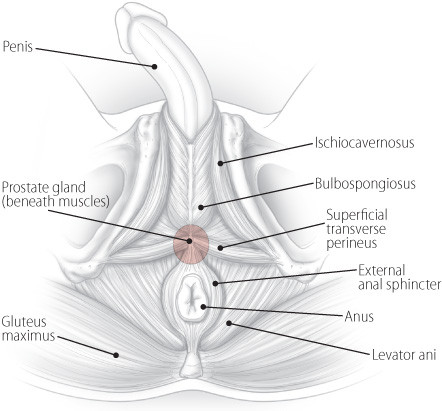
Tightness in muscles that compose the pelvic floor can lead to pelvic pain, often called prostatitis, and difficulty urinating. The pink circle represents the prostate, which lies beneath the muscles.
The doctor prescribed lorazepam (Ativan), a drug often used as a muscle relaxant, and anti-inflammatory medications. He also suggested mild exercise, applying heat to the perineum, and sitting in a hot bath. The lorazepam worked best — just 1 milligram a day relieved James' pain.
A year later, the pain was back. The lorazepam seemed to have stopped working, and urinating was uncomfortable at best. James underwent an ultrasound, an MRI scan, and a cystoscopy, a procedure during which a doctor inserts a device called a cystoscope into the urethra to examine the urinary tract. All the results came back negative. The doctor said that James' pelvic muscles weren't working properly, a condition he called pelvic floor syndrome. He suggested biofeedback, a technique that helps one become more aware of unconscious or involuntary bodily activities so that they can be consciously manipulated.
James saw a specialist in mind-body medicine, but the specialist tried a different technique. "He said, 'You've developed a negative cycle between your brain and your pelvic floor. It's like dealing with chronic pain. You just have to forget about your symptoms. Put them out of your mind. If you have pain, just tell the pain to go away and get on with your life,'" James recalled.
James decided to give it a try. He returned to his exercise routine at the gym. He also resumed having sex with his wife, which he had been avoiding. When he felt pain, he pushed it out of his mind. And for two years, he managed to keep the symptoms at bay.
But one morning in December 2008, James had sex with his wife. Later that day, he was in pain and developed urinary urgency, which sent him back to the doctor. Once again, all of the tests were negative, and once again, the doctor concluded that James had pelvic floor syndrome.
James and his team of caregivers recently spoke about what happened next, his current treatment, and what men with similar symptoms might try to quell the pain and restore their quality of life. These are the caregivers:
- William C. DeWolf, M.D., a professor of surgery at Harvard Medical School and chief of urology at Beth Israel Deaconess Medical Center. He is particularly interested in prostate diseases and urinary tract cancers. He also serves on the editorial board of Harvard Medical School's Annual Report on Prostate Diseases.
- Patricia Jenkyns, P.T., a physical therapist in the women's health physical therapy program at Brigham and Women's Hospital. She has worked mainly with women for the past 25 years, but increasingly, men have been seeking her expertise. She also teaches and trains others to provide pelvic floor physical therapy.
- Anurag K. Das, M.D., an assistant professor of surgery at Harvard Medical School and director of the Center for Neurourology and Continence at Beth Israel Deaconess Medical Center. His areas of interest include incontinence, voiding dysfunction, pelvic prolapse in women, and prostate enlargement (BPH).
You said your symptoms returned in December 2008. What was the pain like?
JAMES: The pain was not as bad as it had been in the past, but I developed problems with urination. I saw Dr. DeWolf a couple of times because I was not able to urinate. I even went to the emergency room because I felt like I had to void, but I was not able to void. It was scary. They did an ultrasound and determined that I didn't have anything in my bladder.
When your bladder was full, were you able to void?
JAMES: Later on, yes. But one day I was not able to urinate for 24 hours. On my way to see Dr. DeWolf, I stopped to go to the bathroom a few times. Things just suddenly opened up, and I was able to urinate. But Dr. DeWolf did a cystoscopy and a urodynamic study, and he didn't find anything wrong. Again, he diagnosed pelvic floor syndrome and suggested that I try biofeedback.
What do you mean by pelvic floor syndrome? What's the pelvic floor?
JENKYNS: The pelvic floor is the whole bony container that surrounds the organs in the pelvis. The pelvic floor muscles are the muscles involved with bowel, bladder, and sexual function. They include the levator ani, bulbospongiosus, ischiocavernosus, and superficial transverse perineus. Pelvic floor syndrome means that these muscles aren't working properly, causing problems with bowel, bladder, or sexual function.
It's quite frightening when pain and other problems affect this part of the body because information about it isn't readily available, and it's not talked about openly. You're not going to walk up to your next-door neighbor and say, "I've got this terrible pain in my scrotum." So people often feel anxious, alone, and helpless.
What training do you have to work with the pelvic floor?
JENKYNS: I started specializing in pelvic floor dysfunction in 1984 with Elizabeth Noble, an Australian physical therapist who formed the Section on Women's Health of the American Physical Therapy Association in 1977. Initially, I treated incontinence in postpartum and elderly women. Soon after that, pelvic floor pain problems were recognized in women, too. We learned through experience. Now I develop course work and provide training to others seeking a certificate of achievement in pelvic physical therapy.
Awareness and understanding of pelvic floor pain — as well as research on treating pain — have continued to grow. Women and men of all ages can be affected. In the last several years, the number of men seeing a physical therapist for pelvic floor work has increased dramatically.
What can you do to help someone like André?
JENKYNS: There are often telltale signs in a patient's history that point to difficulties in relaxing the pelvic floor muscles — straining during urination or bowel movements, for example. In André's case, the accumulation of stress, habitual pelvic floor muscle holding, and poor voiding habits led to an overactive pelvic floor, but it varies from person to person.
So I start by assessing the pelvic floor muscles. Can the patient contract them with ease? Can he relax them with ease? Can he do that consistently? When he bears down, do the pelvic floor muscles lengthen and relax? When he coughs, do those muscles contract with increased intra-abdominal pressure as they should? These functions are visually and manually assessed. In addition, the perineum, skin, superficial muscles, and the deeper levator ani muscles, innervated by the pudendal nerve, are felt for trigger points.
To see which trigger points cause muscle contraction?
JENKYNS: No, I'm looking to see whether touching specific points causes pain. First, the anal sphincter is examined for trigger points. Then, moving farther into the rectum, the levator ani muscles and the prostate are felt for painful trigger points. In André's case, he had pain in his perineum, superficial muscles, and levator ani externally, as well as trigger-point pain in his anal sphincter and levator ani muscles rectally. He could not relax his pelvic floor muscles following a contraction or with bearing down. This is common in men with urinary frequency and urgency and pelvic pain.
How do you address the frequency and urgency issues?
JENKYNS: The patient is instructed to keep a bladder diary for three days in order to find out how often he voids and, if there is urgency, how much urgency. Many people don't interpret the bladder's signals correctly and void too frequently. As soon as they feel any bladder sensation, they think, "I must have to go to the bathroom." Patients need to understand that if they never let the bladder fill completely, it can become sensitive to filling and will lose the capacity to hold urine over time. The average number of voids is five to seven times a day, or every two to four hours. The bladder should allow people to sleep through the night, although voiding once during the night is considered normal.
What is biofeedback? Where does that fit into the puzzle?
JENKYNS: Biofeedback enables a person to become more aware of their body's signals. It is very useful for pelvic floor muscles because they are not visible. With increased awareness, patients can learn to correctly contract, relax, and coordinate these muscles so they work more effectively.
There are different types of biofeedback. Simple biofeedback can be done using your hand or a mirror. Pressure biofeedback can be used to strengthen weak muscles — patients can feel improvement when they squeeze an air-filled rectal sensor. I do not use pressure biofeedback for cases like André's; he needed to concentrate on relaxation. Instead, I use a biofeedback unit with two "channels," so that he can see what is happening in two different muscle groups: the pelvic floor muscles and the abdominal muscles. Ultimately, we want to coordinate the activity of these two muscle groups.
How do you do that?
JENKYNS: One channel detects the activity of the anal sphincter and levator ani muscles through a sensor placed in the rectum. Surface electrodes from the second channel are placed on other parts of the body, such as the abdominal muscles. The sensor and electrodes detect the electrical activity of the muscles, and that information is filtered by the biofeedback equipment [see Figure 2]. It is displayed on a computer screen, with the data reported in microvolts. When squeezing the pelvic floor muscles, you should see an increase in activity on the screen. When relaxing, the activity should go down. If the patient cannot relax his pelvic floor muscles, the electrical activity stays high. With an overactive pelvic floor, the goal is to train the muscles to relax. When the patient relaxes the tight muscles, the electrical output decreases, and the patient can see a lower signal on the screen.
Figure 2: Biofeedback equipment
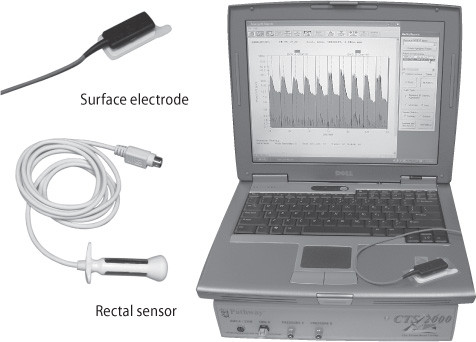
The surface electrode and rectal sensor plug in to a biofeedback machine (beneath the computer). Together, they detect and measure the electrical activity of muscles. Variations in muscle activity during contraction and relaxation are displayed on the computer screen.
What do you ask the patient to do during biofeedback?
JENKYNS: I start by taking a 30-second baseline reading to see what the muscles look like during rest. Then I look at the patient's ability to contract and relax those muscles. I'll ask him to contract 10 times, with each contraction lasting for two seconds, followed by four seconds of relaxation [see Figure 3]. Then I'll ask him to contract for five seconds and relax for 10 seconds. Based on the feedback, it becomes evident what the treatment plan needs to concentrate on. The patient needs to link what's happening on the screen to what they feel in their muscles in order to receive the most benefit from biofeedback.
Figure 3: What biofeedback shows
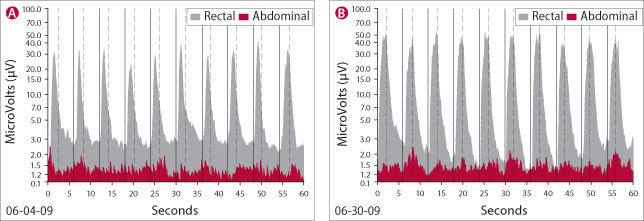
The biofeedback machine produces graphs like these. Tall dark gray bands represent muscle activity in the rectum; low red bands show abdominal muscle activity. The high peaks occur during muscle contractions; valleys occur when muscles relax. Both graph A and B show a series of two-second contractions followed by four-second periods of relaxation. Notice how valleys in graph B deepen as the patient becomes more aware of the muscles' activity. The abdominal muscles are better coordinated with the rectal muscles in graph B — peaks and valleys in both red and gray bands happen at the same time. Practice helps. The session illustrated in graph B took place nearly a month after the session shown in graph A.
And then you try to have the patient reproduce that voluntarily?
JENKYNS: Exactly, but not just reproduce it once. It's essential for patients to reproduce it consistently. That is the key. Habits die hard, so it's important for the patient to practice repeatedly what he's learned in the treatment sessions. Many people with pelvic pain, urinary frequency, and urgency habitually contract the pelvic floor muscles. A helpful exercise is to tune in to those muscles five times a day and voluntarily release the tension in them. Breathing exercises and meditation can help decrease the electrical activity.
Is there medical literature that supports the use of biofeedback for patients with chronic pelvic pain syndrome?
JENKYNS: There is evidence linking pelvic floor muscle spasm with pelvic pain, urinary frequency, and urgency, and some research on the use of biofeedback in men with pelvic pain. The studies show that it is a safe and effective treatment that provides pain relief. We also have anecdotal evidence that it works, but larger randomized clinical trials need to be done to confirm this. [See "Biofeedback for CPPS."]
Biofeedback for CPPS
Clemens JQ, Nadler RB, Schaeffer AJ, et al. Biofeedback, Pelvic Floor Reeducation, and Bladder Training for Male Chronic Pelvic Pain Syndrome. Urology 2000;56:951–55. PMID: 11113739.
Cornel EB, van Haarst EP, Schaarsberg RW, Geels J. The Effect of Biofeedback Physical Therapy in Men with Chronic Pelvic Pain Syndrome Type III. European Urology 2005;47:607–11. PMID: 15826751.
Ye ZQ, Cai D, Lan RZ, et al. Biofeedback Therapy for Chronic Pelvic Pain Syndrome. Asian Journal of Andrology 2003;5:155–58. PMID: 12778328.
Do you think that habitual contraction of the pelvic floor muscles was responsible for André's penile and testicular pain and his urinary difficulties?
JENKYNS: Yes. It is likely that habitual contraction of the pelvic floor muscles led to pelvic floor muscle spasms that caused the pain and urinary difficulties. In terms of urinary difficulties, the pelvic floor muscles need to relax for the bladder to empty. Biofeedback can be used in a variety of positions to promote relaxation. André found that when he lies down and completely relaxes by using diaphragmatic breathing and meditation, he can relax his pelvic floor muscles. He still has difficulty relaxing the muscles while standing and trying to urinate, but he continues to practice. Sometimes, it may be helpful for men to sit down to urinate so that they can better relax those muscles.
DAS: That's actually an issue in women. A lot of women believe that toilet seats are dirty, so they don't want to sit on them to urinate. Instead they hover over the toilet. But you can't relax the pelvic floor sufficiently when you hover. We try to get them to sit or squat — squatting is okay, but you can't hover.
I've seen patients whose pelvic floor muscles are so tight that they even walk awkwardly. You can literally see the tension. Changing that is difficult because it's probably built up over many years. You can't just get rid of it.
JENKYNS: That's why I think André's symptoms have changed over the years. The tension is accumulating and getting worse and worse.
Do you think the testicular pain he experienced back in 1996 is part of the same process that is going on now?
JENKYNS: I think it was an early sign. He's had several flare-ups, and they seem to occur when there's more tension and stress in his life. He manages to let go of some of the tension for a while, but then it flares up again. It's an up-and-down process, and over time, the tension builds.
JAMES: It's definitely stress-related. One day, I heard some upsetting news from a family member. After that, I felt as if there was a foreign object in my rectum. I was convinced that I suddenly developed a rectal tumor. I couldn't even walk because of the pain. I went to my primary care physician, who sent me to have a sigmoidoscopy. [See "What's a sigmoidoscopy?"] That didn't show anything, and eventually the discomfort went away. But now when I have a flare-up of my pelvic floor syndrome, I sometimes experience pain in my rectum.
JENKYNS: I also ask André and the other men I work with to do some lower-extremity stretching to work the hip joints and all of the related muscles.
What's a sigmoidoscopy?
During this test, doctors examine the inside of the rectum and the last section of the large intestine — the sigmoid colon — using a flexible viewing tube inserted through the anus. Doctors use a similar device during a colonoscopy, but they examine the entire length of the large intestine.
And that helps?
JENKYNS: Yes, it can ease the tension.
JAMES: It helps tremendously. I can't overstate the value of stretching. It really helps relax the pelvic floor. After stretching, I can urinate much more easily.
What is myofascial release? Is it done internally? Externally?
JENKYNS: "Myo" means muscle and "fascia" refers to the elastic connective tissue that surrounds and supports the muscles, organs, bones, nerves, and blood vessels in the body. Stress, trauma, chronic inflammation, overuse, and poor posture can cause the fascia to thicken and tighten. So, in general, myofascial release is a type of massage that focuses on desensitizing the nervous system, easing tension, and stretching and lengthening muscles and fascia to relieve pain.
For patients like André, we focus on the pelvic floor muscles and surrounding soft tissues, doing both external and internal work.
With massage?
JENKYNS: Yes. There are different types of massage, also called soft tissue mobilization. Skin rolling is one technique in which the skin is lifted between the thumb and fingers and gently rolled back and forth to release any restrictions between the skin and underlying tissues. In addition, pressure is repeatedly applied along the entire length of muscle or over taut bands of tissue. The amount of pressure varies and depends on the patient's response, but the overall goal is to lessen the pain and quiet down the nervous system.
There is only minimal research on myofascial release for pelvic pain in men, but the few studies that have been done have found it beneficial. In the clinic, I've seen patients improve with myofascial release, especially in combination with biofeedback, stretching exercises, and bladder retraining.
What about prostatic massage?
DAS: That was a therapy for prostatitis in the early 20th century. It was later used to help drain fluids from the prostate so that they could be checked for infection and to help open any blocked prostate ducts — at least in theory. With little else to offer, some doctors are trying this with patients, and some patients do seem to improve.
My theory is that the prostate massage has nothing to do with the prostate. Rather, you are stretching the external sphincter, the rectal sphincter, and other muscles, and that's what helps the patient. I don't think the improvement some patients experience has anything to do with the massage of the prostate itself.
What do you do on a daily basis, André, to keep the pain and urinary problems at bay?
JAMES: Well, in addition to my periodic biofeedback and myofascial trigger point release sessions, I try to stretch. I'm still on lorazepam. And I try to avoid stress, because stress is clearly a trigger for me.
Dr. Das, what role have you played in André's care? How do you treat patients in a similar situation?
DAS: I see a lot of patients with frequency and urgency complaints as well as patients who can't completely void. I tend to see people at the extremes, including patients who can't "go" at all. And I see patients who haven't had success with biofeedback or pelvic floor work. In such cases, I treat them with direct nerve stimulation. This involves electrically stimulating the sacral nerve and sacral nerve root.
To do this, a small needle is placed in the lower back at the third sacral nerve root. [The sacrum is a wedge-shaped set of bones near the base of the spine; nerves travel through gaps in these bones.] Then a wire is placed through the needle and attached to a small electrical stimulator after it's taped securely to the skin. The patient can carry the stimulator, which is the size of a cell phone, on a belt or in a pocket. He or she uses it for a week, keeping track of voiding habits. If the patient feels that his or her symptoms have improved significantly, and we see improvement of 50% of more objectively, we consider permanently implanting the device.
And you are doing this in men?
DAS: Yes. About 10% of our patients with these severe problems are men.
What are the specific indications for implanting a nerve stimulator?
DAS: The three indications from the FDA are frequency and urgency — patients who are going about 20 times a day or almost every hour; urge incontinence — patients who can't make it to the bathroom; and retention — patients who can't go at all.
And the reason they went into retention?
DAS: The theory is that they are not relaxing their pelvic floor muscles. The first thing that occurs when you try to void is that the pelvic floor should relax. If you can't relax the pelvic floor, you can't start voiding.
What gave you the wisdom to send this patient to see a physical therapist for biofeedback, Dr. DeWolf?
DeWOLF: My interest in this started when I was a resident and heard a talk by a famous urologist, Dr. Frank Hinman, about psychogenic retention in pediatric patients. These kids seemed to have complete urinary obstruction, but tests showed nothing was wrong with them. They were eventually cured with hypnosis. Hinman thought that there was a lack of coordination between the external sphincter and the bladder. I filed that idea away.
Then I started to see some patients with what the NIH called type III prostatitis, which is pelvic pain without infection. Urinary symptoms may or may not be present. Applying what I had learned from Dr. Hinman in the 1970s, I started developing a hypothesis that these patients have a pelvic floor that isn't coordinated with how the bladder works. The pelvic floor becomes impenetrable. As Dr. Das just said, the first act of voiding is relaxation of the pelvic floor. If you can't relax it, then the bladder has a hard time releasing urine. That's what I mean by pelvic floor syndrome.
There are several signs that tell me I'm dealing with a patient who has a pelvic floor problem. First of all, the patient will likely be on the young side — in my experience, most patients are between 35 and 50 years old when the problem starts. Second, there will be nothing wrong with the patient's physical evaluation. He can void, and he doesn't get up several times a night to urinate. He doesn't have a urinary tract infection. But because the pelvic floor muscles are tight, he is in pain — and the pain makes the pelvic floor even more resistant to relaxation.
So here's what happens: the pelvic floor tightens up, but the bladder tries to push urine through it. In doing so, it generates high pressures and — this is an important point — it puts very high pressure on the prostate, because the bladder is trying to force urine through the urethral sphincter. Remember, the urethra runs through the prostate. Done repetitively, this can irritate the prostate, causing pain in anything attached or related to the prostate — the testicles, the penis, which is attached to the urethra, the rectum, the suprapubic area, or the bladder. The bladder registers that as urgency, and it becomes inflamed. I used to prescribe muscle relaxants to patients with pelvic floor muscle tightness.
Was there scientific evidence to support the use of muscle relaxants?
DeWOLF: Frank Hinman's original work dealt with hypnosis to relax the muscles. Not knowing what else to do, I tried the pharmacological equivalent of hypnosis. But now I refer my patients for biofeedback and myofascial trigger point release. I tell them that it might take awhile to reverse the problem, but I think it's the only way to attack it. Patients have to learn how to relax the pelvic floor. If they lessen tension in the pelvic floor, the pain dissipates and the bladder can empty normally.
Any concluding comments?
DeWOLF: It amazes me that there are 1.8 million men in the United States who have CPPS, according to the NIH, but it's so poorly understood. There's nothing obviously wrong, nothing to fix, so doctors just refer these patients to someone else. I now see at least one patient a week with this condition, and he's usually been to four or five other physicians before me. I think it's critical that we learn more about this condition and study the effectiveness of different treatments so that we can provide the best possible care for our patients — and help alleviate their suffering.
Originally published October 2009; last reviewed Feb. 23, 2011
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles. No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.
I have been suffering from chronic prostatitis since 2011. I went to several urologists but every one had his own diagnosis.. some said it is nerve pain. Some said inflammation in prostate.. some said it is in ur mind.. during entire period of this chronic disease I was symptoms free twice.. let me share with all you guys that what I did to get relief from painfull symptoms.. after 2.5 years of strating of chronic prostatitis/pelvis pain and no relief from medicine, one day I was laying on my bed with pain in my rectum/anal, I folded a smal piece of toilet paper and put it in my anus with the thought that while walking it may help to avoid rubbing and pain.. but when I put this folded piece of toilet paper in my anus I felt that burning / hot gas came out from anus and sudden improvement in my symptoms.. thereafter most of the time I kept this in my anus and I feel relief.. after one month doing this I was symptoms free and urine follow was normal.. after1.5 years, one day I did masterbation and symtoms came back.. I tried toilet paper stratigy again but this time it didn't work.. It was end of 2014 when my symtoms came back.. In September 2016, I started sitting on my toes while working on my laptop with the thought that it will help to stretch my pelvis area but unfortunately pain started in my knees.. in order to treat my knees pain, I started taking turmaric mixed with boiled milk every night along with supplement called adjoint to get relief from my knee pain.. I also noticed that my urine symptoms were also getting better. I continued taking this herbs about three months and my urine symptoms go down with 90 % improvement.. now after passing 9 months, I again felt some symptoms few days back.. I got ultrasound of my prostate and found that there is urine retention in my bladder after passing urine.. and protate is enlarged.. I consulted with Dr. he told me that prostate size doesn't matter and for urine retention, cystoscopy is advised.. now I started talking turmaric and adjoint supplements again to relief pain.. my story may help some one like me… My opinion is that doctors have no cure of this chronic disease.. we sufferers can share our stories to reach at best possible treatment options
A friend of mine recommended the use of PeaPlex. For a long while, I have also been suffering from Hip complaint. At first, I was a bit skeptic but I am happy she persuaded me. I have been using PeaPlex for about three months now and I feel a lot better! I ordered it via rs4supplements.com.
Recommend all of you one chinese herbal medicine named diuretic and anti-inflammatory pill to relive pelvic-pain, it works well.
You can google more info on it.
Lizzy Cromwell
November 23, 2017
!!!!!!!This is the most wonderful thing i have ever experienced, And i need to share this great testimony, I just want to say thanks to Dr.Mack for taking time to help me cast the spell that brought back my ex husband, last year my husband left me for because things were not working out between us, so he had to call it a quit, my Husband abandoned me, everything was so hard for me, i love him so much, i could not take the heart break, i had to find a solution then i came across Dr Mack On how he has been helping ladies in getting there husband back so i contacted him and he help me to cast a return spell for my husband and the next day my husband left his side chick and he came back to me pleading for forgiveness with so much love and caring. i will never forget this help that DR Mack gave to me. if you are here you need help to get you lover back you can contact him via email——-dr_mack@ yahoo. com………
Great write-up, I'm regular visitor of one's website, maintain up the excellent operate, and It is going to be a regular visitor for a lengthy time.
wretye5ryabcd.com
Laurie Oakes
April 17, 2017
I thought I had IC, but had another dysfunction.
mindovermusclematters.com
Charles Beutt
March 4, 2017
I had pudendal nerve entrapment/Chronic pelvic pain syndrome for 15 years. Nothing worked, pudendal nerve entrapment release surgery, drugs, stretching, relaxing, diet, nothing. I found out about the Graston technique/Astym where a metal bar is run over the skin that breaks up scar tissue under the skin. That done over the abdominals, pubis, lower pelvis, and hamstrings, combined with some internal work to gently stretch the pelvic floor muscles has turned my life around. I also add some deep stretching outside the skin with the point of the metal bar pushed into the angry spasmed muscle/ligament attachments. I feel almost like I should go tell doctors/professionals what worked for me. I had tried everything and saw just about every pelvic expert.
Hi Peter,
Can you share the links of the videos which you have followed in your treatment.
-Neel
Hi All,
After wasted trips to a urologist that couldn't diagnose me with this condition, I finally have cured myself. For me, it was just constant stretching and movement through out the day. Look up YouTube videos for pelvic floor release. I do it every morning and night…and during my workday I sit on a heat pad and do stretches to keep everything loose. It's very time consuming but over time it works. I was going to the bathroom every 30 mins and the anxiety of constantly having to go was really wearing on me. And my sex life with my girlfriend has returned back to the way it used to be before everything started flaring up down there. It was a very difficult time in my life, as any man can attest to, not being able to please your lover makes you feel like less of a man. And I could tell it was frustrating her not only for herself not being satisfied but knowing that my orgasms were painful and awkward.
You have to make a full effort to rid yourself of this pain and continue to do it but it is possible. Believe that there is a cure and it's achievable and it will help. I hope my story helps others in this situation because I know the mental toll of this condition is worse than the actual physical pain.
-Peter
I grew my penis by 4 extra inches using Dr Anaele Herbal Cream, The main reason for buying this was to add to my penis size. My confidence with with my Girlfriend was low. People with average size penises offer advice on getting straight mentally. Its confidence not penis size. etc etc. Well let me tell you. My penis is about average size now and my confidence has gone through the roof. I religiously followed the exercises. and concentrated on one thing at a time i.e making my penis bigger.. There are Tips as well to show you what to do. They are quite tasteful using cucumbers. In the members area there is a lot of good information on premature ejaculation,increasing your stamina, more self control etc. It is like being in a sweaty shop and inundated with everything. You can't try it all in one go. Concentrate on what you want, All thanks to Dr Anaele for his product for i have also used other which never work out. You can reach him Via email ( dranaele.herbalherbs.remedy @ gmail . com )
Alonzo
September 19, 2016
Dear all,
My history is very similar to most of the above. I have been living in this hell for about 8 years with a few quiet periods. I lost my girlfriend and job because of this. I live in Germany (supposedly a medically advanced country), the truth is that even the recognized urologist here don´t know what to do. After trying most of the above mentioned treatments, a very famous specialist here in Munich has given up and sent me talk to a psychologist. This psychologist recommends approaches such as "you should talk to your prostate and listen to his needs, imagine a dialog between you and your prostate". Truth is that I hope one of these days to muster the courage I need to put an end to my suffering. I can no longer go on like this.
Kathy Doherty
September 1, 2016
Hi My name is Kathy D. and I just submitted a comment.
with my story, and a Physical Therapist recommendation
I don't see it here. How can I tell if it went through?
Thx!
Hi I am a female and have suffered with similar symptoms for almost a decade, so I can really relate.
Last year,I finally found a pelvic floor Physical Therapist who was really knowledgeable. She knows not only the pelvic floor but the entire anatomy, very well.
She practices "The Headache in the Pelvis" program if one is interested, and has trained with Dr.David Wise.
She worked on my many trigger pts, which have since reduced.
I won't go into detail on symptoms etc, but I will say that I improved,am able to be active again, and gained back over 25 lbs of weight I'd lost through fear and worry about this disorder, and whether I'd ever heal. The urologist who works with her is the really the first one I've met,and completely gets this disorder. He is very good as well.
I have still have a long way to go, as my tight pelvic floor caused pain with sitting and also some bowel issues, due to the tightness and the medications. I sometimes have the feeling of something being in my anal sphincters even when I am essentially empty. In my case this is all from a tight pelvic floor.
Worry is my biggest enemy.
I want to take medication to reduce this anxiety, but am afraid of constipation, even tho the docs and nurses assure me the med they prescribed won't constipate. After years of this, I've lost trust and am afraid to try new things, as many things back-fired, before I met my physical therapist.
But I know if I could reduce my worry and learn to relax the pelvic floor, it would help me be much closer to pain free..
I would love to learn more about "laser "that someone mentioned and also Biofeedback, as my Phys. therapist doesn't use it. )
I am a mom of 3 teen-aged to early 20s kids. I can't work right now, but hope to soon. Like one man mentioned, I feel my best when distracted by doing something fun! I need to spend my days thinking about something else. I'm praying to find a work- from- home job so I can do that.
If anyone lives in the North Central NJ area and is interested in my physical therapist ..let me know. She and her urologist partner are the best Ive seen. If anyone knows of work from home opportunities could you also pls let me know?
I wish healing and health to all of you!
Thx!
I have pelvic floor dysfunction that has basically ruined my life. After countless misdiagnoses. Yes, I had endo, Yes I have interstitial cystitis caused by urine unable to leave the body, but no one figured it out. I was in a car accident and 1 month later I could hardly urinate. You tell these ass doctor's at age 30 looking healthy and they don't believe u. I hate all of them. After getting surgery for endometriosis I felt much better but then I incurred a fall at work which must have given me more nerve damage. I fell right on my tail bone thanks to some ladie's luggage. My rectum, bladder and stomach were in extreme pain several months after, but at the time I didn't correlate it with the fall. I go to my gyno and he tells me I might have cancer or need a bowel resection. He knew I had a history of endometriosis. He was trying to antagonize me, I still don't know why. He also looked high when he came into my exam room. I lost all trust in him at that point. He told me because I started to use some estrogen that my endo was probably back. He just kept saying all this stuff. I only had one ovary at the time. I told him I was going to go to the cancer center and have my ovary removed. He called me and said he would do my surgery that he is a competent doctor. I never confronted him about being high. Anyway I had a perfectly healthy ovary removed and 5 days later end up with a rectal spasm that still hasn't gone away. I know the fall and surgery instigated it. I'm so worried this will never go away. It definitely isn't as bad as when I first got it but it is horrible after a bowel movement and when I'm sitting. I can't believe I get sleep. Please someone tell me this will eventually lessen up with time. I just want to know there is hope.I think they surgery traumatized the muscle, I pray it heals.
I think its a heat laser it does not burn or cut anything. If they have it to close it gets hot, then they pull it back. It works to soften scars and muscle tissue. Does not hurt at all and takes about a half hour per treatment. She has a laser that was special made to have higher watts. But it is getting more popular with more chiropractors. First treatment was about $250 but well worth it. Wisconsin
Kurt
Would you please elaborate on the LASER treatment. CPPS sufferer for 4 years.
I was diagnosed with pelvic floor tension myalgia 7 years ago. It started about a year after having a TURP on my prostate. In the past 7 years I have had at least 14 flare ups of prostate infection. The pain has been very severe to the point of begging multiple Drs. to remove everything in front. I started with physical therapy internal and external. Had some relief at $500 a hour after insurance paid half. Then tried massage that was better at fraction the cost. My Dr. treatments were multiple very bad drugs that didn't do a thing. Had 3 MRIs CT scans Pain clinic and bone and joint. Only minor relief. A year an a half ago I was told by university urologist there was no other tings to try that have not already been. Only drug that helped was 4 Motrin 3 times a day. Now I am starting to get high sugar in urine with no family history. So most likely getting some kidney damage. A month ago my wife made me try Laser. A local chiropractor does laser on NFL players an Olympic people. It is a high watt laser. After the first treatment my pain was half. After the second it was at %10 after the third it was gone. Still going once a week. And still no pain.
Does anyone know where I can find resources – specifically a list of doctors, that treat pelvic floor dysfunction in men? It seems nearly impossible to find anyone and my boyfriend has suffered for years up to the point of being unable to work. He's been in physical therapy for months with no improvement. 🙁
i could remember having feelings of using the bathroom a lot in my early to mid tweenties. I noticed
the symptoms would come on stronger after periods of heavy sex and masterbation but although I noticed it, it never bothered me that much. I even remember being 25 and getting up to urinate
a few times a night. My wife would joke about it and so would I. Again at the time it was no big deal.
Since that point on I can remember living like that all through my thirties into my early fourties.
I was having an average of 4 ejaculations a week between sex and self pleasuring. Again I noticed I
would get flare ups of urinating a lot especially after days of frequent sex. To the point of going to
the movies and having to urinate twice before the movie would end. Going to a car dealer and using
the bathroom two and three times during the purchase of a new car. Although I would urinate often
it never hurt and always felt I emptied myself completely even though I would maybe go again in
30 minutes. Yet the symptoms never bothered me much becuase I was able to take long car trips with no issues and at times I had no issues at all. I guess since my mind was free of the symptoms even though they were there it was out of sight out of mind. I also was a heavy coffee drinker and diet soda by the tons and thankfully still loved to drink water down like a horse, so I also felt my symptoms were there becuase I was a heavy fluid drinker especially coffee. It's funny how being ignorant sometimes is best. I also would like to add that I have been suffering from anxiety since
my tweenties and went through heavy periods of business stress in my late thirties. Again ignorant to my symptoms of stress and excessive urination at the time. Which brings me to my night mare story. One day three years ago at the age 41 I got this terrible urge to urinate constantly. It was BAD! We are talking every 10 minutes! I would have to urinate constantly but with a super good
flow. I panicked at the thoughts of what could be wrong with me. I was even afraid to go see a doctor. I was so scared yet did not know what to do about it. Fear was my worse enemy. I lived like that for about two weeks with my symptoms getting a little better but still feeling terribly scared and confused. Then one day I decided to drink some alkazeltzer tablets and felt sooooooo much better after a few minutes I was giggling inside with joy. I thought to myself. How could this be? I felt almost 100 percent better. I even woke up the next day still felling better. That was in early November of 2012. I felt better and mostly symptom free for almost two months. It was life as usual and drank what I wanted and had my usual sex of about 4 times a week. Then Christmas Day of 2012 of what seemed to be the start of an amazing Christmas I decided to have some holiday sex with my spouse. It was about two hours later and BOOM! The extreme urge to urinate came back sending me to the bathroom every ten minutes. Again my urine flow was super strong. I went into pure panic! I thought this urine thing was over and here it was back even stronger then before. Talk about a terrible Christmas Day. Again I was terrified of what was going on and did not go see a doctor. I even hid my symptoms from my wife. Tried the alkazeltzer thing, but it was just a band aide of help. I even went off to my family holiday vacation to celebrate the New Year with my wife & 10 year old boy. Don't ask me how but I was able to hide it from my wife and family for a period of two months. Huge mistake! I finally stared to get chills and lower back aches until I broke and asked for help and went to see my family doctor. He told me I had prostitis with out examining me at all, just ordered a urine culture and two weeks if Cipro. I was feeling terrible. Nothing seemed to help. The Cipro did nothing, so went to see another GP who did a full exam on me. DIgital rectal exam, urine, blood work even a EKG becuase I was in panic. My DRE was perfect he said. No sign of anything on my prostate. Urine and blood work all perfect. My PSA was 0.4 that is super good number. Yet my symptoms got a bit better but nothing major. Still suffering even though I was told everything is fine. Two months later I went to see a urologist who saw my other test and told me to take another antibiotic another urine culture uro dynamics test and he checked my testosterone. Came back a week later and told everything was super good and told me to go home and meditate, that I was his healthiest patient! Yet every night my symptoms were at their worst. I felt I couldn't even pee at times. I was miserable and crying like a baby all the time in the shower. I would hide a lot of my feelings from my spouse and would just play them off. As far as she knew I was healthy but was still feeling some symptoms. I needed her to be able move on and take care of my sons needs and daily activities. Although my symptoms went from god awful to border line terrible I was feeling a bit better, but still very frustrated. I did not know was going on. I was in pure panic and depression. I felt the need to urinate even when I did not have to. I remember sitting in my car alone just crying and not knowing what do. After all I was a healthy guy according the doctors. I called my mother one day hysterical and she informed my GP who prescribed me Xanax. I had never taken one in my life. I picked it up from the pharmacy and took .5 mg tablet with water. 30 minutes later I was like WOW! I felt much better and calm. It was like the hand of God saying relax a bit you need it. I would then continue take Xanax as needed but was still feeling all around awful. The only that would help was Xanax and masterbation every 3 days. I was scared to do more as I knew deep inside my symptoms were from over use from excessive ejaculation. The feeling better would only last a few hours after sex and then would just come back. Again thanks to Xanax I was getting by. A year had past and my symptoms although better were still there. I stopped the doctor shopping and went to see a psychiatrist. She did some lab work on me to check my thyroid and vitamins levels as all else had shown to be ok. She kept me on the Xanax and also put me on Lexapro. She was nice and told me to relax. The Lexapro helped my mood, but the Xanax was the big helper. I started drinking red wine again with my doctors consent since my Xanax doses were considered low and noticed I felt symptom free when I drank some wine. Just two or three glasses on a Saturday night would keep me at a gathering or a dinner basically symptom free. Go figure it's diuretic but it's also a depressant so it calmed me down. I was still not feeling 100 percent and my had flare ups here and there that would put me in a panic. I also started taking two baby aspirins a day for preventive health. Because my blood pressure would rise from anxiety and that small dose would along with a Xanax would calm a flare up quick. Still feeling desperate and going on two years of my symptoms I found a women urologist in my area. Yes a women. I felt good with my female psychiatrist so thought a female urologist would listen to me better. Well she did. She was a good listener and I explained everything that had happened. She did urine test, DRE, checked my testicles and lower area for any abnormalities. She did a swab to check for Std. Told me all was ok and to relax and enjoy another upcoming holiday and that their was no sign of infection and to let's wait for the swab results. After the New Year I saw her again and she told me I was negative for everything. I insisted she keep searching so she did another urine test but this time a post prostate massage to see if anything showed up. That test did show a slight infection but just a tad few white blood cells that were of not of any issue. Mostly inconclusive and no need for treatment. Still she put me on two months of levoflacine antibiotic as a precaution. She also gave me some Flow Max to use as needed. I went back after the two months and she did another post prostate massage urine test and this one showed absolutely nothing and she told me their was nothing else she could do but to try other medications to see which one worked for me. She diagnosed me CPPS chronic pelvic pain syndrome also known as chronic prostitis even though all my test showed I was ok. She also recommended I try physical therapy but was not to hopeful about its rate of success. I never tried it because she even said it was a hit or miss, but it might be worth a try. My GP told me not to even bother with the physical therapy that is bs. So I decided to try other medications such as muscles relaxants, bladder medications that did not help or make my symptoms worse. I decided to just stay with the Lexapro and Xanax and insisted on a sonogram and a cystoscopy. The urologist basically ignored me becuase she already felt I was properly diagnosed. So I got an order from my GP and did a bladder, kidney and prostate sonogram. All were perfect. I insisted again for cystoscopy and she finally did it. It was normal with the exception of some smooth veins on one side of my bladder. She said she did not what it was but that it was nothin bad either. She also ordere a urine cytology which checks for cancer cells in the urine. Also negative. A radiologist looked my bladder picture also said they were just veins and he did not see anything abnormal. My GP thinks it's an internal birth mark as I have a bunch of them on my body and highly doubts that it's a cause of my symptoms. The urologist was at her end with options for me and told me to do another cystoscopy is in near future to check for any changes. That's just to cover their butts. Their was no reason to do another one according to my GP especially so soon. He agrees that by symptoms are pelvic pain and stress related. So does my psychiatrist. To day it's been 3 plus years of dealing with this. I am feeling better and better as time goes by but ever so slowly. I am 80 percent better all around and even have days where I feel almost 100 percent. I have sex only once a week as I noticed doing once s week instead twice made me feel and heal all around better even though I feel like want to do it much more. I am still taking Xanax and Lexapro with the occasional minor flare up. My main symptom now is needing tourinate about every hour to hour and a half. Slight feeling of not be fully emptied but not all the time. The days I have sex I feel almost syptom free and maybe be the next day then it's back to 80 percent better. At this stage of this condition I have also developed post traumatic stress from going through this ordeal and my thoughts can greatly control how good or bad I feel. It's like my body has been in war yet it's been with me and nit real enemy. Doctors call thus condition and not disease. It's very frustrating that with today's advances where a patient can have two heart stents put in one day be on medications and take care of themselves and they feel all around ok. Yet men with this type condition are left to deal with it on their own through trial and error. I am thankful to be better and really feel that time has proven to some heel all types of wounds how ever slowly it may occur.
Prostatitis Epididymitis
December 15, 2015
I stumbled across this article (and many, many others), when I was trying to relieve my lingering groin pain, after the antibiotics finished with my Prostatitis.
It was the Yoga exercise that I searched / found, that finally relieved the lingering groin pain. I included the details in my Self Help Blog (Prostatitis Epididymitis Pain).
You can google the blog title "Devil In Your Balls".
I have a post on Sitz baths (which gave me the most pain relief), and Yoga Exercise, CPPS, Ultrasound, ….
It's aimed at those that are searching for information, to help understand their problem. I definitely understand many of your frustrations, when there is "nothing" wrong, but the pain continues.
GL
This was a very good article. Just reading it and knowing that other men struggle with this, really helps. My symptoms began with terrible penis tip/urethra pain in June of 2014. I was prescribed enough different antibiotics to choke a horse. I was tested for every STD, prostate secretion test, several digital exams, all with negative results. I had a scope done also with nothing out of the ordinary discovered. Over the course of 4-5 months I had many urine tests, never once indicating any infection. I saw several local urologists with all of them clueless. The pain continued for about 9 months, waxing and waning, but always there. Then I began to have strange feelings in my penis, sometimes feeling that I had an erection when I didn't, other times just a crawling sensation, very difficult to describe. Then the pain went away and was replaced with a constant need to urinate, with the feeling most pronounced at my penis tip. This has been my most constant issue to date. Some days it's really bad, other times barely noticeable. I finally traveled to The Cleveland Clinic, where based completely on my described symptoms, I was diagnosed with Chronic Prostatitis/Pelvic Floor Dysfunction. I did weekly pelvic floor therapy with mixed results, and discontinued after about 15 sessions. I find that when I travel for vacation, head to our cabin, or visit with good friends that my symptoms almost disappear. I have questioned my sanity many times with this condition. How does the discomfort and pain and urgency disappear for a week while I'm on vacation, only then to return the day we return home? I'm convinced there is a psychological aspect to this, that is completely sub-conscious. I live day to day with this condition, and I realize that I'm in it for the long haul. I am still active, and try to do everything I did before. The trouble is that I think about it every day, hoping for a good day and worried about it. I'm certain that contributes to some of the severity of symptoms. I find it amazing that this condition exists and in our day and age, so few options are available for recovery.
I have pelvic floor dysfunction and I have been amazing ever since I was introduced to a physical therapists who is certified through PRI (Postural Restoration Institution) This is not a joke, after one visit my symptoms had almost completely gone away. The therapy is is based on postural deficits and muscular imbalances. They only do exercises which are meant to turn off overactive muscles and turn on inhibited muscles. They're goal is to get the body back to a neutral posture and then they give exercises so to strengthen the neutral posture, if that makes sense? It has seriously changed my life. I have been symptom free for 8 months. I just do my exercises and the pain stays away. I had all of the symptoms. Pain after ejaculation, pain during ejaculation, sensitivity at the tip of my penis and thr base of it, left testicle was swollen and red, pain above my left public bone (which was probably the most annoying). I had problems voiding, feeling of always needing to go, pain during urination. I also had this sensation of something crawling over my scrotum (never compression I'm assuming). But I don't have any of it anymore. There is hope. Before I met the PT certified in PRI I had seen my PCP, Urologist, and someone who specialized in Pelvic Floor Dysfunction. I got no where with any of them. This really may be hard to believe but it really only took one visit for me to feel exponentially better. I don't work for these people at PRI so please if you're not getting better then find someone who is certified through them. They don't massage muscles or give stim, nothing like that. They focus on the whole body to find out where the problem is coming from. You'll see, good luck and stay positive.
Will HMS please update the article with any connection of the pelvic pain to erectile dysfunction? The latter is the most serious thing to worry about.
I can sincerely sympathize with all those who have CPPS. I had an enlarged prostate for years and was having many night trips to the bathroom and difficulty urinating. Finally went to a Urologist. He put me on Flomax and I saw about a 25% improvement and was fairly satisfied with that. Uro said he could make it a lot better with green light laser TURP surgery and make me pee like I was 20 yrs old. Well, I believed him and had the surgery. BIGGEST MISTAKE OF MY LIFE!! I was much worse after the surgery and that's when my CPPS started from the nerve damage done by the laser and trauma to the area. I was told by the Uro that I was just a slow healer and it would eventually get better. 7 months later, I went to my summer home in WA. State USA and saw a 2nd Uro. He did a cystoscopy (my 3rd one) and said there was definitely room for improvement. I discovered that Doctors have a special code, that they don't negatively criticize each other. 2nd Uro did a 2nd TURP surgery with a different type laser called "button plasma". After 6 week recovery, I could pee like a 20 year old but still was getting burning in urethra area, prostate area, rectal area and pain radiating throughout my pelvic area all off and on all never in the same place. 2nd Uro DID vastly improve my life but pain was not gone. My family doctor started me on hydrocodone then oxycodone that helps a lot but has side effects. Since my 2nd surgery, I've also seen Gastro. drs. and went to the Wise/Anderson CPPS seminar in Santa Rosa CA. Aug. 2014 which was 6 days, expensive, but worth it. I saw Dr. Wise's Urologist there and he also said and confirmed what other Doctors had said, that my CPPS was nerve damage from to hot a laser or done incorrectly and it could or could not get better in time, everyone is different. Since then I went to another Gastro for the rectal pain and had colonoscopy done that turned out normal. He also said, pain was probably nerve pain from damage done from 1st TURP back in Jan. 2013. He put me on Gabapentin for the nerve pain which does help some as it stopped the pain I was getting in my left testicle. So now I'm on meds for the pain, Gabapentin, Oxycodone and Rapaflo which is to keep the urethra open and clear. I can pee very well but still have good and bad days. Been over 2 years since this all started. Before I had my 1st surgery, all I did was pee a lot but no pain and sex was good and frequent at least 2-3 times a week, and I was 67 yrs old at that time, now 70. Sex now is not so good maybe 1 time every 2 weeks because I usually hurt for a couple days after and have retrograde ejaculation from the TURP surgery. As far as help, the best I've found so far and with no risk is the Wise/Anderson protocol. It can help although I have not kept it up like I should. According to Dr. Wise, it is not uncommon for CPPS to take 1-2 years before significant improvement. DR. Wise DID have CPPS himself for over 20 years and DOES KNOW what we have and are going through and understands with a lot of sincerity and sympathy. Give him a call and talk to him. He is very approachable and a doctor dedicated to help us with CPPS any way he can and a real regular guy. Hope this helps you guys and get well.
Mandar Paranjpe
March 2, 2015
I am an ophthalmologist, suffering from burning sensation around my distal urethra for last 3 months. I have consulted an urologist who diagnosed pelvic muscle spasm. He also prescribed Tamsolusin, which I could not tolerate(tachycardia). Please suggest some treatment for pain relief. I travel for about 150 km everyday( have a driver to drive). I also have h/o low back ache for many years.
Hello. I am in a state of confusion. I'm not sure if I have cpps or pudendal neuralgia. Can they overlap. I definitely suffer from pelvic pain with urinary symptoms of pain with my bladd er filling and pain on my penis. But The most frustrating symptom that no one else has mentioned; erectile dyafunction with decreased sensation
Moe. You need to try reverse kegels. Kegel exercises will only make your PE worse.
thank you for your article. great read! amazing anatomy and explanation. keep em coming….
hi,
I am having a lot of problems trying to cope with my willy pain. I'm at breaking point here and if nothing happens to help I will castrate myself. Any responses would be greatly appreciated.
Many Thanks
J balls
hi,
I am having a lot of problems trying to cope with my willy pain. I'm at breaking point here and if nothing happens to help I will castrate myself. Any responses would be greatly appreciated.
Many Thanks
J dog
hello ? im waiting an answer for my question below please?
i would like to comment a very important point about this. hoping someone might help me and contact me in private. my story started , i used to have erection all the time at least 2 minutes a day and it stands, my friend advised me to do kegel exercise because i was suffering from premature ejaculation, i did it for 4 months. suddenly everything changed , i don't have erection at all , and once i have it , i have it very weak and soft , ejaculation very fast , prostatius problems , higher WBC but no bacteria in semen culture. i thought it is phsycological , but since i forgot this totally but now it stays with me for a year so im sure it is not. i did all tests from penile doppler to all things are fine. doctors don't know what i should i do, so i think this is the reason i might make my musceles more tight. im living in United Arab Emirates and they don't have good physiotherapist. so can someone help me to cure this thing in me and what to start with , i can even pay him or her as if im consulting a real doctor i really need help on this im feeling phsyco and sick because sometimes i feel i have no pennis . what should i do please help
Finally, a relevant article. I have been searching for years for something that reflects what I am going through. The frustrating thing is the periods of normalcy. I'm just coming out of one. It was fine for several weeks and now I'm in the throes of another attach. I undergo regular physio therapy and it has been helpful in firstly identifying and also, to some extent, dealing with it. I have learned techniques to relax the area but nothing permanent so far. When this all started I thought it was hemorrhoids and even endured a hemorrhoidectomy. The strange thing it was fine for almost a year after that but then came back with a vengeance. My concern is that my case has also started to affect my sex life. Often, during intercourse, I have a sharp pain that almost feels like ground up glass in my rectum – burning almost but very localized. Hard to explain. Also, not sure if it is connected, I've been having issues with my left testicle as well. The eppiditymus has "hardened" it seems. I see a urologist at the end of the month.
Tough to read of all the suffering. I have it too. 9 years and counting, and all I can say is acceptance while fighting the good fight is the only way to survive this psychologically. Like Tom, I haven't had a relationship in a long time, and actually lost my last one because of this condition. We're forced to quickly change our expectations of ourselves and what life has to offer us. Better than the alternative, I guess.
I don't understand what is going on. I feel like the entire left side of my pelvis/hip area is under pressure from something inside. My left testicle has been retracted all the way to the opening of my inguinal canal for over a year. Under additional mental or physical stress, it retracts into the canal itself. My pelvic floor irregularly throbs or shivers for hours on end. Much of the time, I have difficulty urinating. One of my doctors did say he thought my prostate was enlarged, but what if it's because the tight muscles I feel in my pelvis are putting pressure on it?
I've taken rounds of bactrim, cypro, and ibuprofin. I'm now on finasteride and prozac (for depression). The thought of sex terrifies me because orgasm is so painful during, and for days afterward. Nothing feels like it is functioning normally in that part of my body. I don't want to date anyone and part of me doesn't want anyone interested in dating me (because I don't know what is wrong with me!).
I've been suffering with these kinds of symptoms for over 1 year. It's terrible, and I feel like my whole life is on hold. It is so difficult to concentrate on anything for long periods of time. All I can do is try to maintain my sanity as the hours pass as I go about my routine from week to week. I'm terrified of living this way for the rest of my life, and I want to defeat this, but the medical professionals I've been to seem very puzzled by my case, and I have not felt like they were taking me entirely seriously. I can't seem to get anyone, for example, to believe me when I say that my testicle has literally bee dislocated for over a year!
My story is almost exactly to James! I was taught to do exercises which helped however lately symptoms have returned…. I changed my workouts and think the stress if weightlifting irrates it. But I don't want to stop training!!! Whate exercises and stretches can I do besides pelvic floor squeezes ????
For the past 8 months or so, I have what feels like a tightening of mussels in my rear end. I have a problem with urinating and the Dr. feels it is related to the prostate. However, although it may be slightly enlarged and I do get a slight feeling of a lump I do not feel it is causing this hurting pain and very tight mussels that I can't release. I wonder if it is also coming from the anal sphincter mussel. My PSA score is 1.27 and no signs of cancer. I was taking a tramadol which gave me some relief but that is diminishing. What could be causing this and who should I see. The urologist says nothing about this tightening of mussels and wants to do surgery on the prostate. I also mentioned this to my PCP and again he just passes it on. I'm tired of going and explaining to doctors and still have the hurting pain or tightness which I believe is causing the pain.
@Mike
For the men out there with this horrendous condition, I would suggest reading 'End Male Pelvic Pain' by Isa Herrera (see 'End Female Pelvic Pain' if you are a woman with this type of pain). It offers good exercises, stretches, massage techniques, breathing & meditative techniques, and advice for sufferers of pelvic pain & pelvic floor dysfunction. After having suffered a car accident, I found this book to be invaluable to alleviate my pain
I forgot to ask: for those of you here who are experts with the pelvic floor muscles, are they are any aerobic exercises I can do that will not disturb that area? I desperately need to exercise, but everything I try seems tighten my pelvic floor.
I've noticed that I get the pain when I have sex or masturbate. The pain will last for days…. mostly in the pelvic region. I think a good diet can also help.
Can I still have sex when I have CPPS?
Dear Tom,
I am sorry to hear that you have been suffering with this condition for as long as Ive been alive. That is horrible…God bless you for being able to cope with the pain for so long. There is a solution that I am in the process of doing. Its called the Stanford Protocol it was developed by a psychologist by the name of Dr. Wise. He uses a combination of physical therapy and meditation. You should also try muscle relaxants, they are helpful because this is a condition that has to do with muscle tension and taut bands forming which lead to trigger points that need to be pressed to relieve symptoms. The website you can learn more about it is here: pelvicpainhelp.com. I hope the best for you, by the grace of God I hope you will be healed.
Tom Demyan
October 26, 2014
I have suffered from what finally was diagnosed by me to my Dr. as CPPS….I have had all of the symptoms which began 25 years ago, yes in 1989. The thought of sex starts some of the symptoms, but after having sex, I'm hurting for weeks. Solution: I've been single the past 17 years and that hurts even more. I have tried all medications and herbs, but now just sit on an ice pack most evenings. Sometimes I get so depressed. Is there anything new out there to try? Tom
Just a note.
The intervention by the "specialist in mind-body medicine" was ludicrous! Hardly an authentic mind-body approach.
Rob Menasco
November 28, 2013
I just wanted to say that frontline urologist are 10 to 30 years behind the timeline presented in this article. I spent the better part of last decade taking Cipro and it wasn't until I talked to them and I
Saw my internist put me on lyrica for fibromyalgia that all my symptoms went away.
I don't even have a urologist here in DC.
Commenting has been closed for this post.
, Urinary Urgency and Frequency and Feels Like a Rubber Band Around My Low Back and Groin Area ?
Source: https://www.health.harvard.edu/blog/finding-help-for-pelvic-pain-a-patients-story-20090203212
0 Response to ", Urinary Urgency and Frequency and Feels Like a Rubber Band Around My Low Back and Groin Area ?"
Post a Comment